
Getting involved in sports from an early age has a myriad of benefits. It gets kids active, builds on their teamwork skills, forms new friendships and is great for their strength building and coordination – among the various other mental, physical, social and emotional benefits.
We think that the Novak Djokovic Foundation words the benefits very well:
- Kids’ character and moral principles are formed through fair play
- Sports experiences help to build positive self- esteem in children
- Sports bring people together from all over the world, regardless of their nationality, religion, culture, or skin colour
- Teamwork and benefits of social interaction among children are best seen in sports
- Playing sports enables them to create friendships they otherwise might not have formed
- They view competitions on and off the field as opportunities to learn from their success and failure
- They learn to respect authority, rules, team colleagues and opponents
- Sport is an important learning environment for children
- Participating in sports can be a helpful way of reducing stress and increasing feelings of physical and mental well-being
While any and all sports will help to harness these important skills and experiences, we at Perform Podiatry thought we’d shed some light on a question we occasionally get asked by parents around which sports are best for certain areas and stages of development. We thought we’d break it down by age category and the activities and functions that are typically learnt and built on within the age range.
Preschool Age
At this age, kids are still getting their feet planted firmly on the ground and are developing a good grasp on their coordination, balance and general motor function. At this age, it’s important to focus more on mastering the basics and less on ‘joining a team’ or looking at competing, if it’s just for the sake of it anyway.
Swimming, dancing, running, side to side movements, catching, throwing and activities that look at improving balance and coordination, both at the feet/legs and the hands/arms, are encouraged. We remember playing bullrush and other games at preschool that while were played with others, thinking back on them now, really focused on developing each person individually as opposed to focusing on the team dynamics that become more important in the next age range. Spending time throwing and catching with your kids at this age can provide just as much (if not more) value, growth and development, so make the most of this time together.
Primary School Age
This is the time that kids can really enjoy and benefit from team sports and organised activities. They’re at school and building important social skills and a good understanding of how a team operates together. Mentally, they’re getting stronger and have a greater focus and drive. Physically, they’re also getting stronger and can run further for longer, throw better, and the like. They will have developed good coordination and at this age will pick up almost any sport with great ease, working on the skills particular to that sport, if they enjoy it that is.
You can’t go too far wrong with the sports offered at primary school, some of our favourites include netball, tennis, cricket (and generally all bat/ball sports), soccer, handball, basketball, touch rugby, running and the like.
It’s also a great time to start getting involved in activities like gymnastics, swimming and martial arts where you have a greater focus on yourself as part of the team and start honing new skills.
Intermediate School Age
There is a lot that happens during this time and age that has an effect on kids in sport. Kids start to get quite good, confident and skilled in the sports they’ve been playing or participating in for the years leading up to this. Part of this is their improved memory and understanding of techniques and strategies involved in sport, as well as their improved physical strength, speed, size and general ability.
With this age comes growth spurts and unfortunately, for some kids, that also means growing pains. This means more time and care needs to be taken on warming up, cooling down and general conditioning of muscles.
This is the age that kids also start getting involved in contact sports such as tackle rugby, that may have previously not been suitable due to inadequate strength in bones and muscles and hence a higher risk of injury. This does need to be considered on a case-by-case basis, as every child grows and matures at varying times.
Alongside all of the previously mentioned sports, kids can start more technical sports like hockey and volleyball, if they haven’t already tried it sooner.
High School Age
At this age, the world is their oyster! They have good, refined motor skills that have built up over the last eight years. Kids (though they’re not so much ‘kids’ anymore) can pick up sports relatively quickly, especially if they’ve had experience playing similar sports. We remember starting sports like fencing and underwater hockey at high-school, both of which utilised the technical skills from various other sports and activities.
Growing pains and growth-related injuries can still occur so be mindful and make sure your kids get the right treatment and adequate rest/recovery if they develop pain or injury.
If you have any questions about this, are worried about your child’s development, or they’re experiencing pain or injury, give our team a call on 09 523 2333 or book online! We’re the kid’s foot experts in Auckland, located at the One Health Building on Remuera Road, close to Newmarket.
 The symptoms of flat feet aren’t necessarily painful themselves, but the stress and pressure they put on the surrounding tendons and structures can cause pain as tendinopathies and other issues develop. These tend to be exacerbated by long periods of time on the feet and high-impact activities.
When podiatrists evaluate the severity of flat feet, they often look for signs as opposed to symptoms. These include:
The symptoms of flat feet aren’t necessarily painful themselves, but the stress and pressure they put on the surrounding tendons and structures can cause pain as tendinopathies and other issues develop. These tend to be exacerbated by long periods of time on the feet and high-impact activities.
When podiatrists evaluate the severity of flat feet, they often look for signs as opposed to symptoms. These include:
 On our end, we conduct a comprehensive biomechanical assessment in which we:
On our end, we conduct a comprehensive biomechanical assessment in which we: Getting involved in sports from an early age has a myriad of benefits. It gets kids active, builds on their teamwork skills, forms new friendships and is great for their strength building and coordination – among the various other mental, physical, social and emotional benefits.
We think that the Novak Djokovic Foundation words the benefits very well:
Getting involved in sports from an early age has a myriad of benefits. It gets kids active, builds on their teamwork skills, forms new friendships and is great for their strength building and coordination – among the various other mental, physical, social and emotional benefits.
We think that the Novak Djokovic Foundation words the benefits very well:
 Have you noticed that two of your toes have come out of line? Perhaps where they used to line up normally alongside one another, they’re now moving apart from one another like a ‘V’. This is actually something we refer to as the ‘
Have you noticed that two of your toes have come out of line? Perhaps where they used to line up normally alongside one another, they’re now moving apart from one another like a ‘V’. This is actually something we refer to as the ‘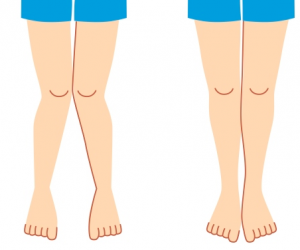 We love seeing kids here at Perform Podiatry. Partly because it’s hard to be away from our own and they brighten up our day, but largely because of the massive difference that we know we can make to their lives and development.
Kids should be able to run, play, explore, learn and have fun without being limited by pain or held back by foot or leg dysfunction. Thankfully, issues that arise in kids are usually much easier to manage than in adults. Today we thought we’d share on a condition that we’ve had a few questions about lately from concerned parents – knock knees!
We love seeing kids here at Perform Podiatry. Partly because it’s hard to be away from our own and they brighten up our day, but largely because of the massive difference that we know we can make to their lives and development.
Kids should be able to run, play, explore, learn and have fun without being limited by pain or held back by foot or leg dysfunction. Thankfully, issues that arise in kids are usually much easier to manage than in adults. Today we thought we’d share on a condition that we’ve had a few questions about lately from concerned parents – knock knees!
 A lot of us have heard that it’s not uncommon to have a slight difference in the size of our feet or even legs. We often advise patients to buy shoes to the size of the larger foot so that toes don’t get cramped and cause pain. But when it comes to having a slight difference in the length of the legs, does it make any difference or have any effect on the body? Let’s start with the basics about limb length discrepancies.
A lot of us have heard that it’s not uncommon to have a slight difference in the size of our feet or even legs. We often advise patients to buy shoes to the size of the larger foot so that toes don’t get cramped and cause pain. But when it comes to having a slight difference in the length of the legs, does it make any difference or have any effect on the body? Let’s start with the basics about limb length discrepancies.

 When you come in contact with the fungus and your immune system doesn’t clear the infection before it takes hold, the symptoms will begin. Certain conditions do make people more susceptible to infection. These include:
When you come in contact with the fungus and your immune system doesn’t clear the infection before it takes hold, the symptoms will begin. Certain conditions do make people more susceptible to infection. These include:
 Arthritis – it can be painful, frustrating and limiting for many New Zealanders. In fact, almost 50% of those aged over 60 years, and almost all over 80 years old, are affected by osteoarthritis arthritis in New Zealand. Yep, that means that if you haven’t already, you and your family members have a high chance of developing arthritis as we age!
Often, arthritis is perceived to have limited treatment options because of its degenerative and irreversible nature. The truth is that while you can’t reverse the damage from osteoarthritis, we definitely have tools to help ease your pain and improve your comfort!
But first, let’s start with the basics.
Arthritis – it can be painful, frustrating and limiting for many New Zealanders. In fact, almost 50% of those aged over 60 years, and almost all over 80 years old, are affected by osteoarthritis arthritis in New Zealand. Yep, that means that if you haven’t already, you and your family members have a high chance of developing arthritis as we age!
Often, arthritis is perceived to have limited treatment options because of its degenerative and irreversible nature. The truth is that while you can’t reverse the damage from osteoarthritis, we definitely have tools to help ease your pain and improve your comfort!
But first, let’s start with the basics.
