
Author: Hanan Kane


Caring For Your Ingrown Toenails After Nail Surgery
If you’ve recently had an ingrown toenail surgery and are wondering how to optimise your recovery, here are some quick tips that we let our patients know about after their procedures.
Immediately after your procedure
- Take the rest of your day off from work, school and any physical activity commitments. You want to kickstart the healing process and reduce the risk of continued bleeding
- Keep your foot elevated as much as possible for the rest of the day
- Use paracetamol if you need to manage pain, as opposed to ibuprofen, which can thin the blood
- Don’t get your foot wet, shower with your foot completely waterproof, or wait until the next day to shower
- Keep your foot clean, and don’t remove your dressing
- Don’t drive on the day after your procedure
- Don’t wear closed-in footwear on the day of your procedure
Within the first week of your procedure
- Return within 2-3 days for your dressing change
- After your redressing with us, redress your toe every 1-2 days, or anytime that your toe gets wet
- Don’t remove or play with your dressing before your first dressing change
- Don’t get your toe or dressing wet, if you do, let us know and we may get you in earlier to redress your toe
- Avoid wearing tight shoes and socks that push on your toe
- Avoid any activity that causes toe pain
- Take time to elevate your foot where possible
- Avoid any physical activities that involve kicking and direct impact to the toe
The first one to two weeks
- Return for your one week check with us, where we’ll be able to check the status of your healing and debride if needed
- At this stage, different people may be at different healing stages, so it’s important to listen to the advice of your podiatrist
- Continue to redress your toe as instructed. We’ll let you know when you can switch the kind of dressing you use to one that is less rigorous
- Be cautious during physical activity until your toe has healed sufficiently
- Continue to avoid any activities that cause you pain
- Wear open-toed shoes as much as possible to encourage healing
- Let your podiatrist know if you are experiencing significant pain, or are worried about infection
After two weeks
At this stage, your toe should have healed sufficiently to not be bleeding or leaking any white or yellow fluid. This means that you should be able to continue with a simple dressing to cover the toe, as opposed to heavier absorbent dressings. Many people will now be able to return to regular physical activities and wearing regular shoes. We do not anticipate that you will be experiencing significant pain. If you do, continue to use paracetamol as directed. Depending on your health and other medical conditions, it can take anywhere from 2-8 weeks for complete healing. If you’re worried about your progress, give us a call.

How Can Orthotics Relieve Pain From My Foot?
Orthotics are one of the most common treatment methods we use with foot pain and injury, due to the fantastic results we can achieve with them. If you’re not very familiar with orthotics, you may wonder how orthotics can help with so many problems – and how they work.
Today, we’re talking about a very important feature of orthotics – their ability to offload pressure. While orthotics have a myriad of other features that help them achieve their desired function (i.e. to help you recover from your injury and get pain-free), we’re going to start bringing you into the world of orthotics right here.
What you must know about orthotics
Before we start, we must emphasise this about our orthotics. The orthotics that we prescribe for you are custom-made for your feet, your pain, your injury, and the individual characteristics of your feet. These are not the one-size-fits-all silicon inserts you grab from the pharmacy in the hopes that you’ll feel more comfortable. Your orthotics are designed and made for you, using decades of knowledge and experience.
This is why an item that is under the broad term of ‘orthotic’ can achieve so many effects for many different people – every pair is different. Much like prescription glasses, they can help with many problems. Also, like prescription glasses, there’s a big difference between the ones you pick up at the supermarket, and the ones you get from your optometrist.
Off-loading – what does it mean?
When we talk about ‘offloading pressure’, we mean removing the pressure that is being applied to an area of your foot that is causing you pain. For example, say that your big toe joint at the ball of your foot is swollen and painful. Anytime your foot hits the ground, that joint has pressure applied to it as you push against the ground and you feel pain. In fact, because the joint is swollen, it is probably taking on even more pressure than it was previously.
Off-loading would mean redistributing the pressure away from this big toe joint, and instead, spreading it evenly between the lesser joints of the ball of the foot. These non-painful joints then take on a little more pressure each, and the big toe joint is either partially or completely offloaded, letting it heal – while you experience significantly less pain with every step.
How does an orthotic off-load pressure?
The real answer is – any way we design and prescribe it to! There are many offloading features that we can incorporate into an orthotic. Taking the example above, we can do a cut-out specifically beneath the big toe joint and the area of pain and swelling. This removes the pressure directly beneath it, using a cushioning top layer on the orthotic to redistribute that pressure over the lesser four toe joints, while helping them absorb some of that impact. This way, these joints will be the ones ‘pushing off’ the ground, instead of the big toe joint, letting it heal.
Taking a different condition as another example, let’s say that you have a neuroma. A neuroma presents as a painful, palpable, pebble-like mass that can develop between your metatarsals (the long bones of your feet). It’s actually the inflammation of the lining of one of your nerves. When you walk, and your metatarsal bones squeeze on the neuroma, you feel pain. We can place a dome-like addition into your orthotic, that sits just behind the position of the neuroma. This will raise the bones on either side of the neuroma, effectively increasing the space between the bones (so they don’t squeeze the neuroma), while removing excess pressure from it while you walk.
How do I know what orthotic will help me best?
Well, truthfully – you don’t. There’s no one-size-fits-all, especially when you must consider how adding a certain feature to your orthotic will affect the other bones and joints in your feet, especially when you have other medical conditions and problems. But that’s where we come in! We perform a comprehensive assessment and get to know you and your history extensively before we prescribe your orthotics.
Then, we’ll design, create and fit your orthotics, monitoring you to ensure you are getting the results that we both want. If you need help with foot pain from an experienced podiatry team, book your appointment online here or call us on (09) 523 2333.

Here’s Why Being Pregnant Made Your Feet Bigger
It’s not a myth. Pregnancy really can and does make women go up in shoe size, and unfortunately, for some women, their feet stay bigger too. This phenomenon can be confusing, after all, why can your foot size increase when you’re pregnant but not when you put on weight? Today, we’re sharing exactly why.
A hormone called ‘Relaxin’
When you’re pregnant, your body is flooded with a number of different hormones. One of these is called relaxin, and it’s responsible for helping to soften and loosen your ligaments and tissues. This is essential as your body is constantly growing and expanding to accommodate your growing baby. Without softer ligaments, this process could be very painful.
Aside from helping the ligaments and tissues in your abdominal area expand, it also affects your feet, as well as the rest of your body. You have a lot of ligaments in your feet that are responsible for keeping bones stable, held in position, and supported. As these loosen, your foot may ‘relax’ and flatten – especially with the increased weight and pressure they’re under. This can result in both an increased width and length of the foot, as well as a generally ‘flatter’ foot.
This is why your feet generally do not increase in size with weight gain (unless there are other factors involved), but do in pregnancy.
Can I prevent my feet from changing size?
Unfortunately, there’s not a lot you can do to prevent hormones from flooding your body and having this effect. What you can do is keep your feet supported throughout your pregnancy. This includes:
- Wearing comfortable, stable and supportive footwear
- Using custom orthotics to support and promote the natural shape and contours of your feet
By keeping your arch supported, you can help limit the stretching of the ligaments on the feet. Having your feet supported with shoe and orthotics can also help prevent overuse injuries from muscles and tendons of the feet and legs having to work harder to keep you moving with a flatter foot position.
Your shoes will also help restore some stability that may be lost with looser ligaments. A good example is ankle sprains – with the ligaments supporting your ankle not being as ‘firm’ as they originally were, you may have a higher risk of ankle sprains. Wearing good, supportive shoes that cup the ankle can help prevent this.
Wear the right size shoes
If your feet have gone up in size and width, make sure you get shoes that fit your new size and don’t try to squeeze into your previous pairs. Trust us, as parents ourselves, the last thing you want with a new baby is foot pain. Invest in new comfortable shoes to limit any rubbing against the sides of your feet, and pressing up against the front of your toes.
Returning back to your original foot size
While some people will return back to their original foot size, others won’t. It’s hard to predict – and even harder to control. Our best advice is to keep your feet supported and protected throughout your pregnancy.
Need help staying comfortable on your feet?
Our experienced podiatry team would love to help. We’re parents too – so we totally get it. You can book your appointment online by clicking here or call us on (09) 523 2333

Treating In-Toeing In Kids
The position of your children’s feet can either keep them free to run and play, or encourage them to trip, fall and result in pain. In-toeing affects many kids as they learn to walk confidently. At a young age, in-toeing may not be an issue – as long as it doesn’t cause other problems and pains. When in-toeing continues into the primary school years, it could indicate that it’s not going to resolve on its own- and help is needed to prevent it from continuing into adulthood.
So why does in-toeing develop and what can you do about it? Today, we share our easy and effective solution to correct in-toeing in kids: the gait plate.
In-toeing: Quick low-down
In-toeing, which is often referred to as pigeon-toeing, can affect both children and adults alike – although adult in-toeing is usually a result of childhood in-toeing not being treated. It’s very easy to spot because of the inward rotation of the feet.
While it may appear like a funny or wobbly walk, the reality is that in-toeing:
- Can cause tripping and falling (and hence painful injuries)
- Indicates an irregularity within the structure or positioning of the bones of the lower limbs
- May be a precursor for further problems and pains
It is typically caused by one of three ways:
(warning, we’re about to get technical here)
Metatarsus Adductus describes the inwards curve of the forefoot (toes) on the rearfoot (heel). This may be described as a ‘banana-shaped’ foot and is thought to be a result of the position of the baby in the womb, so is typically present at birth.
Tibial Torsion is the inward rotation of the shin bone, otherwise known as the tibia. Because the tibia is turned inwards, so is the ankle and foot, resulting in in-toeing. Here, correcting the position of the shin bone will correct the in-toeing.
Femoral Torsion is the inward rotation of the thigh bone (femur). This also rotates the shin bone and the foot, causing in-toeing. You’ll often notice the knees turn in to face one another, too. This is one of the reasons that children are discouraged from sitting in the ‘W’ position – because it rotates the thighs inwards.
Introducing the hero solution: The gait plate
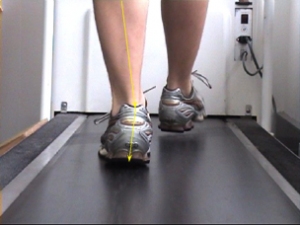
A gait plate is a special type of orthotic that encourages the feet to turn outwards and hence straighten with every step in the shoe and orthotic. It is designed very specifically to the landmarks of a persons’ foot, which is captured with a cast impression following a comprehensive assessment. It works by encouraging the outward rotation of the feet with every step. The orthotics replace the liner of your child’s shoe, and can be moved from shoe to shoe. The best part is – kids can’t even tell that they’re there!
That means no tears and frustration (for both kids and adults!), just pop your shoes on and go.
Worried about the way your child is walking?
We’re parents too – and we’d love to help. To book in with our experienced podiatrists, you can call us on 09 523 2333, or book online here.

Worried About The Way Your Child Is Walking?
“And what is the problem that your daughter is having with her feet?”
“She’s walking funny. I don’t know if it’s normal – it doesn’t seem quite right”
That right there is a conversation that our receptionist has on the phone many times a week. Parents notice that something isn’t *quite* right with the way their kids are walking, and aren’t sure what they should do. Primarily, they don’t know if it’s a normal part of their kid’s growth and development – or whether something isn’t right and their kids may be vulnerable to problems down the track.
This is a very real concern – and as parents ourselves, we want to help. So today, we’re sharing five common problems we see in kids with the way they walk – and what it means for their foot and leg health.
1. Toe Walking
Toe walking describes walking regularly on the balls of the feet, without the heel coming into contact with the ground. It is not uncommon to see this up to the age of three, where kids are still very much exploring walking styles and learning what feels comfortable for them.
Toe walking before the age of three isn’t an indicator of a problem – kids may just be having fun walking this way. It may become a problem if the frequency of this walking style is so high that muscles adjust to this position. As the Achilles tendon remains contracted when on the toes, if it becomes permanently contracted, then kids may have no choice but to continue walking on their toes as attempting to make ground contact may become uncomfortable or painful.
If your child is toe walking beyond the age of three, or they are complaining of any pain or discomfort while toe walking, we recommend bringing them in for an assessment.
2. In-Toeing
Often referred to as pigeon-toeing, in-toeing is the position where the feet turn it to face one another. While the position itself is not typically painful, it can cause kids to trip over their feet and fall more often, leading to other injuries. It may also make them appear clumsy and uncoordinated.
When in-toeing persists beyond the age of four, it’s important to find out the cause. If in-toeing is not present at birth and develops, it is likely caused by the internal rotation of either the shin bone (tibia) or the thigh bone (femur). In this case, it is not just the foot that is affected, but the muscles around the legs, as well as the knee joint.
We’ve been working with a lot of cases of adult in-toeing lately – that is, in-toeing that never resolved in childhood and has persisted into adulthood. While some in-toeing may resolve over time, in others it can persist. If your child is in-toeing past the age of four, bring them in for an assessment.
3. Flat Feet
When your child is first born, they’ll likely have flat feet – and this is completely normal. Their feet will have a big fat pad and no strong, defined foot muscles yet – so don’t worry about whether an arch is forming until your child is at least a couple of years old.
As kids grow and become confident and strong walkers, we do expect that an arch will start to develop. Around the age of four to five is when we’d expect to see a ‘normal’ arch. If it hasn’t developed by the age of five, and they’re not exhibiting any painful symptoms in the feet or legs, then it is likely that they have a flatter foot posture. This means that they may not develop any more of an arch as they grow.
For some children, they may exhibit few symptoms of their flat foot type, other than some tired or achy legs on days that they’re very active on their feet. For others, however, their flat foot posture may make them vulnerable to foot and leg problems. Specifically, they may sustain more overuse injuries as a result of their muscles working harder to support their feet.
If your child still has flat feet at the age of seven, or they develop any pains or aches at any age after they start walking, bring them in for a foot health check.
4. Knock Knees
Knock knees describe the position where the kneecaps turn in to face one another, bringing the knees closer together (and often the feet wider apart). While knock knees around the age of three or four may be a normal part of the development process, they should resolve by the age of seven.
While kids are still young, their knock knees may help them to feel more stable and balanced on their feet. However, when they start to run quickly and participate in sports, knock knees may cause them to trip and fall, injuring themselves.
If knock knees persist beyond the age of seven, or only develop around the age of six, bring them in for an assessment. This will also help rule out any underlying disease.
5. Limping (or other exaggerated hip movements)
If your child starts limping and is in pain, bring them in straight away. If they appear to be limping (or strangely moving their hips or legs) and are not exhibiting any painful symptoms, there are a number of possible causes that we recommend investigating. These include a leg length difference, hip muscle weakness, juvenile arthritis, neurological problems and more.
In these cases, we always recommend an assessment as the safest precautionary measure because limping (or exaggerated hip movements) are not a part of regular growth and development in kids.
Need To Book In With A Children’s Podiatrist?
We love helping kids and families get back to being happy, healthy and feeling great on their feet. We work extensively with children in the Auckland region and have a family-friendly clinic for kids to enjoy. We’re parents too – so we completely understand your fears and concerns.
You can book your appointment online here or call us on (09) 523 2333

Auckland School Holiday Activities 2020
School holidays are here and that means one thing: frantically finding activities that ditch the screen time and embrace the outdoors!
We’re parents too, and we (like many others) are seeking (physical) activities that will also ensure the kids will have a good, long sleep. We found a good bunch for our kids here in Auckland – so thought we’d share them with you too so you *may* be able to enjoy finishing a cup of hot coffee for the first time in years. Disclaimer: We haven’t managed it just yet.
Sculpture in the Gardens
This is an exhibition hosted at the Auckland Botanic Gardens and is now open daily (8am – 6pm) to the public for this Summer right through until Sunday 1st March, 2020. This 2km sculpture trail is absolutely free (yessss) and a great opportunity to get out and about to let the kids explore and complete activities as you all walk around admiring the large scale artworks. While you sip on a hot takeaway coffee. You can find more information here https://www.sculptureinthegardens.nz
The Enchanted Walk
The Enchanted Walk in Alberton on Mt Albert Road is another goodie. Walk around the pathways looking for all the hidden fairy doors and houses dotted throughout. Complete with a bring and swap painted stone garden, this will provide lots of fun for the whole family (because the kids will love it, and you can relax and snap some great pics of the kids to give to your parents for Christmas). Open 10.30am – 4.30pm, Wednesday to Sunday through until the end of February 2020. Find all the information you need here https://www.neighbourhoodarts.org.nz/the-enchanted-walk
Splash Pads
Splash Pads are such a hit during the hot summer months in our books too! Great opportunity for the kids to get out and run around, cool down and have a whole lot of fun while doing so! A great list of some of the best ones in Auckland can be found here https://www.aucklandforkids.co.nz/playgrounds/the-best-splash-pads-in-auckland-for-kids/
Climb to the summit of Rangitoto Island
We like this one because ferries + picnics + walks + views = great family day out! We plan on doing this one with friends that also have kids – and are looking forward to it! For information on ferry crossings and how to get around once you are there, find the Rangitoto Island website here http://rangitoto.co.nz
Local bush walks
There are so many goodies in the Auckland area, so you don’t have to drive far. We plan on showing the kids some photos of things they may find in the forest, so they can look for them and hopefully appreciate the little details of what our beautiful country has to offer! We love this curated list of walks that we found here: http://epiclittlemissions.co.nz/auckland-walks-short
And some more!
We loved finding this list of activities to do these school holidays, but we won’t be forgetting our good-old-faves, such as:
- Heading to the Auckland Zoo for a day out. Aaaand it has a South East Asia Jungle Track opening soon!
- Exploring the Auckland Museum, the Auckland Domain and the Auckland Wintergardens – just keep an eye on the kids around those geese!
- Finding new awesome playgrounds. In our books, it’s an easy winner! https://www.aucklandforkids.co.nz/top-10-playgrounds/
And if your kids have any pains or niggles this summer…
… Bring them in to see our experienced podiatrists! We love helping kids stay happy and healthy on their feet. You can book your appointment online here or call us on 09 523 2333

Is Your Ingrown Toenail Oozing Clear or Yellow Pus? It’s Probably Infected
- Why the risk of developing an infection once you have an ingrown toenail is high
- What you can do to prevent an infection before it develops
- How you can treat your ingrown toenail and infection once it has occurred
You Have A Significant Risk Of Developing An Infection. Here’s Why
 Let’s clear something up: ingrown toenails and infections are not a case of the chicken and the egg – the ingrown toenail comes first.
What classifies a sore toe as an ‘ingrown toenail’ is the moment that the sharp piece of nail goes from merely pushing against the surrounding skin, to actually piercing it and penetrating it.
Think about that for a second – you have a piece of nail that is now constantly inside the skin through a cut down the side of the nail. Every time you walk and move, it’ll move slightly with vibrations of pressures from shoes and socks. Ouch! This also means that while a normal cut occurs and then can heal, this cut can’t – because the ingrown toenail is still constantly piercing it and so keeping the cut open.
An infection occurs when bacteria and other nasties enter the body. Usually, our skin is a fantastic barrier, so while there may be many nasties around us regularly, they never have an ‘in’. Until now. And especially at the ground where you may walk barefooted. And when you give it a perfectly placed entrance – there’s a strong chance that the infection will take hold and start to develop.
Once the infection takes hold, it means increased swelling, pain and oozy discharge (and maybe blood) that is yellow/green/clear in nature and may ‘crust over’.
Let’s clear something up: ingrown toenails and infections are not a case of the chicken and the egg – the ingrown toenail comes first.
What classifies a sore toe as an ‘ingrown toenail’ is the moment that the sharp piece of nail goes from merely pushing against the surrounding skin, to actually piercing it and penetrating it.
Think about that for a second – you have a piece of nail that is now constantly inside the skin through a cut down the side of the nail. Every time you walk and move, it’ll move slightly with vibrations of pressures from shoes and socks. Ouch! This also means that while a normal cut occurs and then can heal, this cut can’t – because the ingrown toenail is still constantly piercing it and so keeping the cut open.
An infection occurs when bacteria and other nasties enter the body. Usually, our skin is a fantastic barrier, so while there may be many nasties around us regularly, they never have an ‘in’. Until now. And especially at the ground where you may walk barefooted. And when you give it a perfectly placed entrance – there’s a strong chance that the infection will take hold and start to develop.
Once the infection takes hold, it means increased swelling, pain and oozy discharge (and maybe blood) that is yellow/green/clear in nature and may ‘crust over’.
Preventing An Infection From Your Ingrown Toenail Before It Develops
So how, then, can we prevent – or at least reduce the risk – of developing an infection? It’s quite simple, really. And no – no Epsom salts required just yet! As the cut from ingrown toenail creates an ‘in’ for the bacteria to take hold, the way to prevent an infection is to remove this ‘in’. This means removing the penetrating nail edge so that the cut can heal, close, and no longer be vulnerable to the infection. Simple, right? – Absolutely.So How Do I Treat My Ingrown Toenail – And The Infection If I Already Have One?
 The best way to ensure the proper care of your ingrown toenail is to see your Podiatrist. Our team here at the Ingrown Toenail Clinic are Podiatrists that are trained in simple and painless ingrown toenail surgeries, as well as conservative care where we safely remove that small, pesky nail edge in a matter of minutes. You’ll feel the relief almost instantly!
We don’t recommend trying to cut back the nail at home because often the nail runs much deeper than you can see, so most people will miss removing the complete penetrating edge and their pain will only continue to worsen. You also won’t have the right tools for the job – whereas we have everything needed to do it quickly and easily – even anaesthetic if you need or want it! (though most people don’t).
Once the sliver of nail is removed, the body will be able to effectively heal the wound and fight the infection – and of course, we’ll help it along by dressing it with betadine (antiseptic). You’re welcome to soak it in some Epsom salts too – but once the nail is out, it should be relatively simple and straightforward for it to heal and the infection to subside.
No more painful, swollen discharge – hooray!
The best way to ensure the proper care of your ingrown toenail is to see your Podiatrist. Our team here at the Ingrown Toenail Clinic are Podiatrists that are trained in simple and painless ingrown toenail surgeries, as well as conservative care where we safely remove that small, pesky nail edge in a matter of minutes. You’ll feel the relief almost instantly!
We don’t recommend trying to cut back the nail at home because often the nail runs much deeper than you can see, so most people will miss removing the complete penetrating edge and their pain will only continue to worsen. You also won’t have the right tools for the job – whereas we have everything needed to do it quickly and easily – even anaesthetic if you need or want it! (though most people don’t).
Once the sliver of nail is removed, the body will be able to effectively heal the wound and fight the infection – and of course, we’ll help it along by dressing it with betadine (antiseptic). You’re welcome to soak it in some Epsom salts too – but once the nail is out, it should be relatively simple and straightforward for it to heal and the infection to subside.
No more painful, swollen discharge – hooray!
Auckland’s Ingrown Toenail Experts
Perform Podiatry are proud to be home to the Auckland Ingrown Toenail Clinic – specialising in the safe and effective care of ingrown toenails – and we do a really good job of it! From simple and easy care to quickly remove the small nail edge, to minor nail surgery to permanently correct ingrown toenails, we’ve got you covered. You can book online here or give us a call on (09) 523 2333.
What Having One ‘Slightly Shorter Leg’ Really Means For Your Body – And Pain
How limb length differences cause you pain
Picture yourself standing straight with one leg being longer than the other. The short leg will be completely straight, and the longer leg will have to bend slightly to compensate for the difference. Your pelvis will be tilted, and the stabilising muscles and ligaments around your hips and pelvis will eventually get used to this tilted position and adjust accordingly. The muscles and alignment of your back will be affected, and the way that you walk will be affected. The longer left leg will have to perform a compensatory movement when it straightens to avoid hitting down into the ground as you walk. You may hike your hip upwards or move the leg out and around as you swing through your step. As your body compensates and starts moving and using muscles differently, your risk for straining and overloading muscles and joints increases. For those whose leg length differences are big enough to cause symptoms, they may experience:- Hip pain
- Back pain
- Knee pain
- Muscular strain and tendinopathies
- Uneven loading and pressure distribution between the legs
 How big does the difference need to be to cause pain?
How big does the difference need to be to cause pain?
There is no universal value for how many millimetres of difference causes you pain. It varies from person to person and depends on your body, too.
In our clinic, when we suspect a limb length difference because a patient has come to us with pain, we usually measure a difference of at least ~6mm. With this said, we’ve also seen patients with a 6mm that don’t experience any symptoms.
To confirm that you have a limb length difference, after identifying a notable difference in our clinic (we wouldn’t classify anything less than 3-4mm as ‘notable’), we then refer you for a scan where your bone lengths will be measured radiographically. You’ll receive the precise difference in limb length, and this will help to direct your treatment.
What can be done to help painful leg length differences?
Treating a leg length difference includes both helping to correct the difference, and treating any problems that it has already caused. We start with a comprehensive biomechanical assessment to find out exactly what muscles have been affected so that we know how to best direct your treatment. We often use custom-prescribed orthotics to help correct the difference by adding a raise to the orthotic for the shorter leg. This helps to equalise the leg length when wearing the orthotics and bring the pelvis and joints back into alignment. We can also make modifications to your shoes to add height to the shoe on the shorter leg. We’ll then work to help rehabilitate any painful and strained muscles that have become damaged because of the leg length difference. Our goal is to help you stay healthy, happy and pain-free not just now but also for the years to come. To book an appointment with one of our experienced Podiatrist, you can call us on 09 523 2333 or book online here. We’re located at the One Health building on Remuera Road, just up from Broadway, Newmarket.
Why Not Having Your Orthotics Checked Every Year Can Put Your Feet At Risk
1. Regardless of how long you’ve had them, your orthotics are working every day.
 Whether you realise it or not – your orthotics are constantly under a lot of pressure. To be precise, you’ll be exerting at least all your body weight over both orthotics – and when you’re running, this can increase to 3 – 4 times your body weight.
Gradually, this can lead to the wear down and compression of your orthotic materials, which affects their ability to provide the support, control and function that they were designed to – and initially would have.
Just like how you’d sharpen a blunt knife so it could keep working effectively, it’s important to check that your orthotics are still doing their job. If they’re not, it doesn’t mean that you’ll always need a completely new set of orthotics. Sometimes, it’s simply a matter of replacing the top cover, reinforcing the control of your orthotics or replacing your pad or addition. You won’t know until you have them checked – and it can be as quick and easy as a 15min check appointment!
Whether you realise it or not – your orthotics are constantly under a lot of pressure. To be precise, you’ll be exerting at least all your body weight over both orthotics – and when you’re running, this can increase to 3 – 4 times your body weight.
Gradually, this can lead to the wear down and compression of your orthotic materials, which affects their ability to provide the support, control and function that they were designed to – and initially would have.
Just like how you’d sharpen a blunt knife so it could keep working effectively, it’s important to check that your orthotics are still doing their job. If they’re not, it doesn’t mean that you’ll always need a completely new set of orthotics. Sometimes, it’s simply a matter of replacing the top cover, reinforcing the control of your orthotics or replacing your pad or addition. You won’t know until you have them checked – and it can be as quick and easy as a 15min check appointment!
2. If your orthotics helped alleviate your original symptoms – how would it affect your life if they came back?
Orthotics are not an ‘on-the-whim’ purchase. They’re a medical device and an investment into your health and mobility for the years to come. They have a very specific function that was prescribed and created by a foot health professional with years of experience in relieving symptoms and improving quality of life. This function may be to stop your foot rolling in and flattening so much, as it was irritating your posterior tibial tendon or plantar fascia and causing pain down the inside of your foot and ankle or the heel. It may be to provide additional stability to your foot and ankle as you’d suffered repeated ankle sprains and had developed some chronic ankle instability along the way. It may have been because your high-arched foot was lacking the shock absorbing function it needed to keep your feet from feeling sore and tired after a long shift on your feet. Whatever the function – if your pain was alleviated (or at least significantly reduced in the case of arthritic pain) by your orthotics, then there’s a good chance that without the adequate support and control from your orthotics, that this pain can come back. And it’s not only the pain that comes back. Pain happens for a reason. It’s a sign that something is wrong – that an injury has occurred – and the pain is a by-product of the damage. When your pain comes back, it means an injury has again occurred and that’ll take time to heal and for the pain to go, even after you repair or replace your orthotics. And that can take a significant toll on your quality of life!3. Your foot structure and position, along with your bone and muscle strength and function, change over time. Your orthotics may need to too.
 As with everything in our lives, we are always changing – and so are our bodies. Our muscles may grow stronger or weaker. Certain medications or events may affect our tissues and the way they function. Our feet change, but they do so very gradually, at a rate that we may not be able to notice. So while we may presume that our feet are the same today as they were 3 years ago, there’s only one way to find out – and that’s to have them checked!
When you come in for an orthotic check, we assess the function of your orthotics against both the reason you needed your orthotics in the first place, and against your feet in their current state. The ultimate question that we look to answer is:
As with everything in our lives, we are always changing – and so are our bodies. Our muscles may grow stronger or weaker. Certain medications or events may affect our tissues and the way they function. Our feet change, but they do so very gradually, at a rate that we may not be able to notice. So while we may presume that our feet are the same today as they were 3 years ago, there’s only one way to find out – and that’s to have them checked!
When you come in for an orthotic check, we assess the function of your orthotics against both the reason you needed your orthotics in the first place, and against your feet in their current state. The ultimate question that we look to answer is: